Staff Training & Billing Support (Complete Guide) Stepwise 2026 Guide — by LifeCareBilling
Billing doesn’t usually fail because a practice “doesn’t care.” It fails because people are busy—and the revenue cycle is made of small steps that must stay consistent even on the busiest days.
A practice can have great providers, a full schedule, and a hardworking team… and still struggle with slow payments, rising denials, and growing A/R. The root cause is often simple: staff are doing their best, but they were never given a clear, repeatable billing workflow to follow.
This guide explains how staff training and billing support should work in 2026—so your team stops reacting to denials and starts preventing them. And throughout the guide, you’ll see how LifeCareBilling supports practices in New York (including Long Island) and nationwide with training, structure, and day-to-day revenue cycle support. (Informational guidance only, not legal advice. Payer rules vary—always confirm payer-specific requirements.)
Why staff training is the “missing lever” in denial reduction
Most billing issues are not “complex problems.” They’re repeat problems. The same handful of errors show up again and again: patient info mismatches, eligibility gaps, missed authorizations, documentation that doesn’t support coding, claim edits, late follow-up, and unclear patient balances.
When staff aren’t trained on one shared standard, each person builds their own version of “how we do billing.” That creates inconsistency—and payers punish inconsistency with rejections, denials, and delays.
Good staff training doesn’t mean turning everyone into an expert coder. It means making sure each role knows exactly what to do at their step so claims move cleanly from visit to payment.
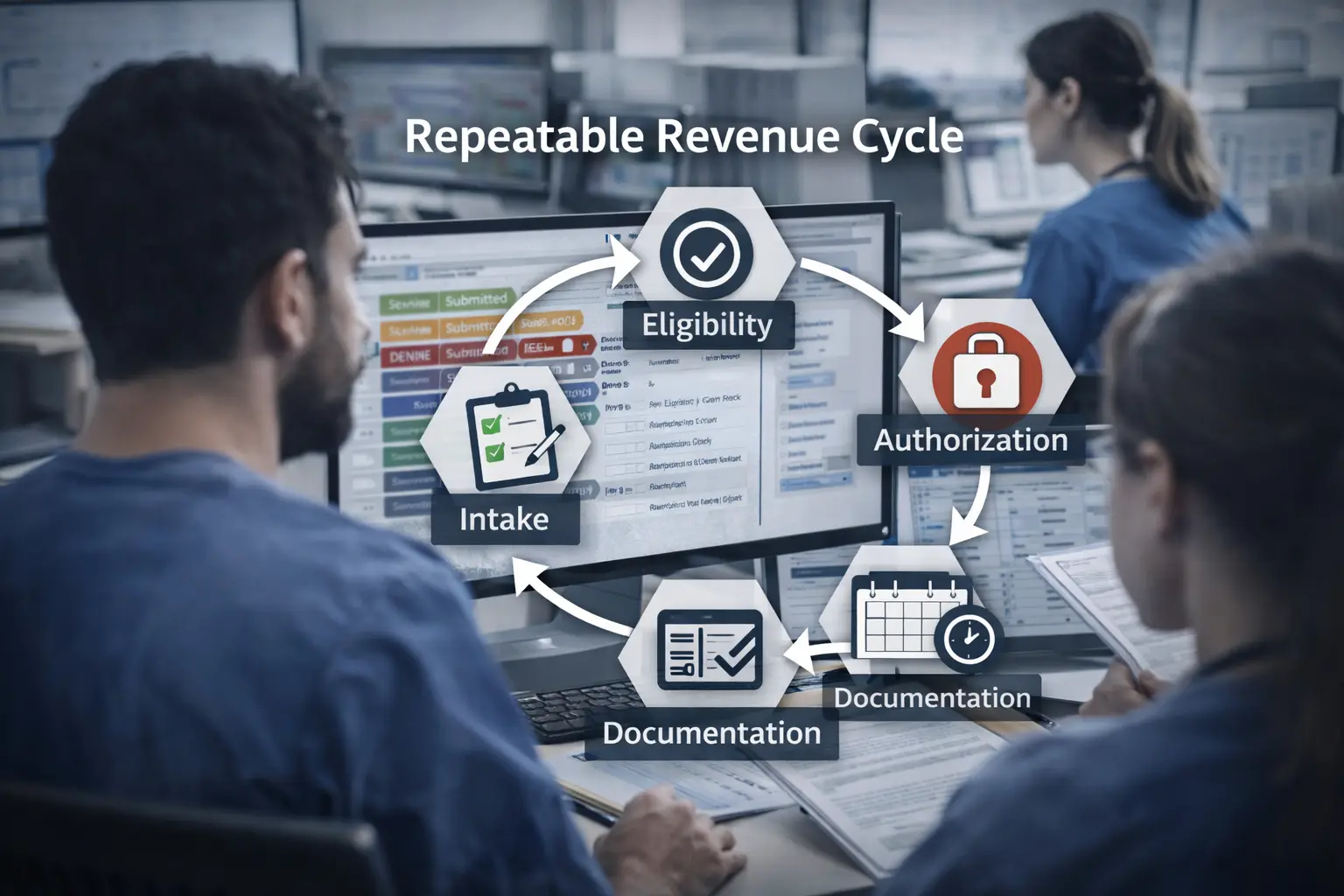
The real goal: a repeatable revenue cycle workflow, not “more effort” Staff training works when it creates structure:
The front desk captures intake correctly every time. Eligibility verification is done deeply enough to prevent avoidable denials. Prior authorization is treated like a gate, not a guess. Providers document consistently for the services you actually bill. Claims submission is clean, and follow-up is disciplined. Denials become feedback, not emergencies.
That’s how you reduce denials, lower Days in A/R, and stabilize cash flow without burning out your team.
Step 1: Start with SOPs and checklists (so training becomes permanent)
Training fails when it lives only in people’s heads. The first step is creating simple SOPs (standard operating procedures) and checklists for each role:
Front desk: registration + insurance capture checklist Billing team: claim preparation + clean claim checklist Authorization: prior auth + referral checklist A/R follow-up: claim status + escalation checklist Payment posting: ERA/EOB posting + variance checklist
When your SOPs are clear, onboarding becomes faster, new hires ramp up quicker, and performance doesn’t drop every time someone is out.
Step 2: Train scheduling + registration (small details that cause big denials)
Most “billing problems” begin with intake.
Staff training here should focus on what payers reject quickly: Correct patient demographics Correct subscriber vs patient relationship Accurate member ID and group number Plan type selection (wrong plan = wrong payer rules) Correct rendering and billing provider identifiers
When this step is strong, claims aren’t born broken—and your billing team stops wasting time fixing preventable errors weeks later.
Step 3: Train eligibility verification the right way
Eligibility verification isn’t just “active coverage.” It’s “will this payer pay for this service with this provider under this plan?”
Training should cover: Network status confirmation (provider + location) Benefit verification tied to visit type/service Referral rules and PCP requirements Deductible/copay/coinsurance expectations (patient responsibility) Flags for authorization needs
This step reduces denials and also improves patient collections, because the patient is less surprised later.
Step 4: Train prior authorization and referral workflows (stop guessing)
Authorization denials are painful because the visit already happened.
Staff need a clear rule: if a service often requires prior authorization, the practice must treat authorization as a pre-visit gate. Training should include: How to identify services commonly requiring auth by payer How to document authorization numbers and validity dates Where to store proof so it’s retrievable for follow-up How to handle referral requirements consistently
This one improvement can eliminate a major category of avoidable denials.
Step 5: Train documentation habits that support coding (without making notes longer)
Providers don’t need “longer notes.” They need consistent notes that support what is billed.
Training should focus on: What documentation elements protect the billed level Common documentation gaps that trigger downcoding or medical necessity denials Clear habits around time-based billing (when relevant) Consistency across providers for the same visit type
This is where billing support becomes valuable: your team shouldn’t be guessing what “good documentation” means for common services.
Step 6: Train coding basics for accuracy (CPT, ICD-10, modifiers)
Even if providers don’t code, staff should understand the basics that drive denials: CPT/HCPCS code selection patterns ICD-10 diagnosis specificity and linkage Modifier logic (a missing modifier can change payment) Common payer edits you see repeatedly in your specialty
The goal is not to replace coders. The goal is to reduce preventable mistakes and improve clean claims on the first pass.
Step 7: Train clean claims and claims submission discipline
A clean claim is the fastest claim. Staff training should cover: Pre-submission validation (required fields, payer rules, provider info) Clearinghouse edits and how to fix rejections quickly Claim submission tracking so “sent” doesn’t mean “done”
When submission is consistent, fewer claims fall into silent delays that later turn into denials.
Step 8: Train payment posting and underpayment awareness
Many practices think the job is done when the payment arrives. That’s where revenue quietly leaks.
Training should include: Correct ERA/EOB posting Adjustment basics and write-off rules How to spot underpayments and patterns by payer When to escalate for correction or appeal
This is how you protect revenue that would otherwise disappear into “close enough.”
Step 9: Train denial management like a feedback loop (not firefighting)
Denial management becomes expensive when the team fixes denials individually but never stops repeats.
Training should include: How to categorize denials (eligibility, auth, coding, medical necessity, timely filing) How to document resolution steps How to identify denial trends by payer/provider/service How to prevent recurrence by fixing the upstream step
This is denial prevention in real life: less rework, fewer repeats, better cash flow.
Step 10: Train A/R follow-up routines (the discipline that stabilizes cash flow)
A/R follow-up is not optional if you want stable revenue. The training goal is simple: every claim has a next action and a date.
Staff should learn: How to work A/R aging buckets How to check claim status and document outcomes When to escalate payer outreach How to avoid “waiting too long” risks (including timely filing windows)
Disciplined follow-up keeps claims from aging into losses.
What “billing support” should look like (when it’s done professionally)
Billing support is not just “someone submits claims.” It’s an operating system around your team.
Strong billing support includes:
- Role-based training and onboarding for new staff
- Clear SOPs and checklists that reduce mistakes
- Ongoing quality checks (spot audits, trend reviews)
- Denial trend reporting and workflow fixes
- A/R follow-up support and escalation handling
- Monthly performance visibility (denials, Days in A/R, first-pass acceptance)
How LifeCareBilling provides staff training and billing support (New York + nationwide)
LifeCareBilling helps practices build a billing system that runs consistently—even when the practice is busy, short-staffed, or growing.
We support you by:
- Training staff by role (front desk, billing, authorization, follow-up)
- Standardizing workflows with SOPs and checklists
- Improving first-pass acceptance through cleaner submissions
- Reducing denials by fixing repeat root causes
- Running disciplined A/R follow-up so revenue doesn’t sit and age
- Providing reporting clarity so owners stop guessing
We support practices in New York (including Long Island) and nationwide. If you want to see where your workflow is leaking revenue—and what to tighten first—start with a clear review.
Call (631) 966-1755 or click Get Free Billing Analysis to see how LifeCareBilling can help you reduce denials, lower Days in A/R, and stabilize cash flow in 2026.
Frequently Asked Questions
What is medical billing staff training?▼
It’s role-based training that teaches front desk, billing staff, and providers how to follow a consistent revenue cycle workflow—so claims are cleaner, denials drop, and payments arrive faster.
Why do practices need revenue cycle training if they already have a biller?▼
Because billing performance depends on multiple roles. If intake, eligibility, authorizations, and documentation are inconsistent, the best biller in the world will spend their day fixing preventable issues.
What should staff training cover first to reduce denials?▼
Start with front-end intake accuracy, eligibility verification, and authorization workflows. These are the highest-impact areas for preventing avoidable denials.
How does billing support help reduce Days in A/R?▼
By keeping claims moving: clean submission discipline, fast correction of rejections, structured follow-up on stalled claims, and denial trend fixes that stop repeats.
How often should billing training happen?▼
Onboarding for every new hire, plus refreshers monthly or quarterly depending on claim volume and denial trends—especially when payers or policies change.
Can LifeCareBilling train our staff without replacing them?▼
Yes. Many practices keep internal staff and use LifeCareBilling for training, workflow structure, quality checks, and follow-through support to improve performance.
What’s the biggest mistake practices make with staff training?▼
They train once, then stop. Without SOPs, checklists, and ongoing feedback, staff drift back to different “personal workflows,” and denials return.
Does staff training help patient collections too?▼
Yes. Better eligibility checks, benefit confirmation, and consistent patient responsibility workflows reduce confusion and improve collection rates.

 Back to Blog
Back to Blog January 9, 2026
January 9, 2026



