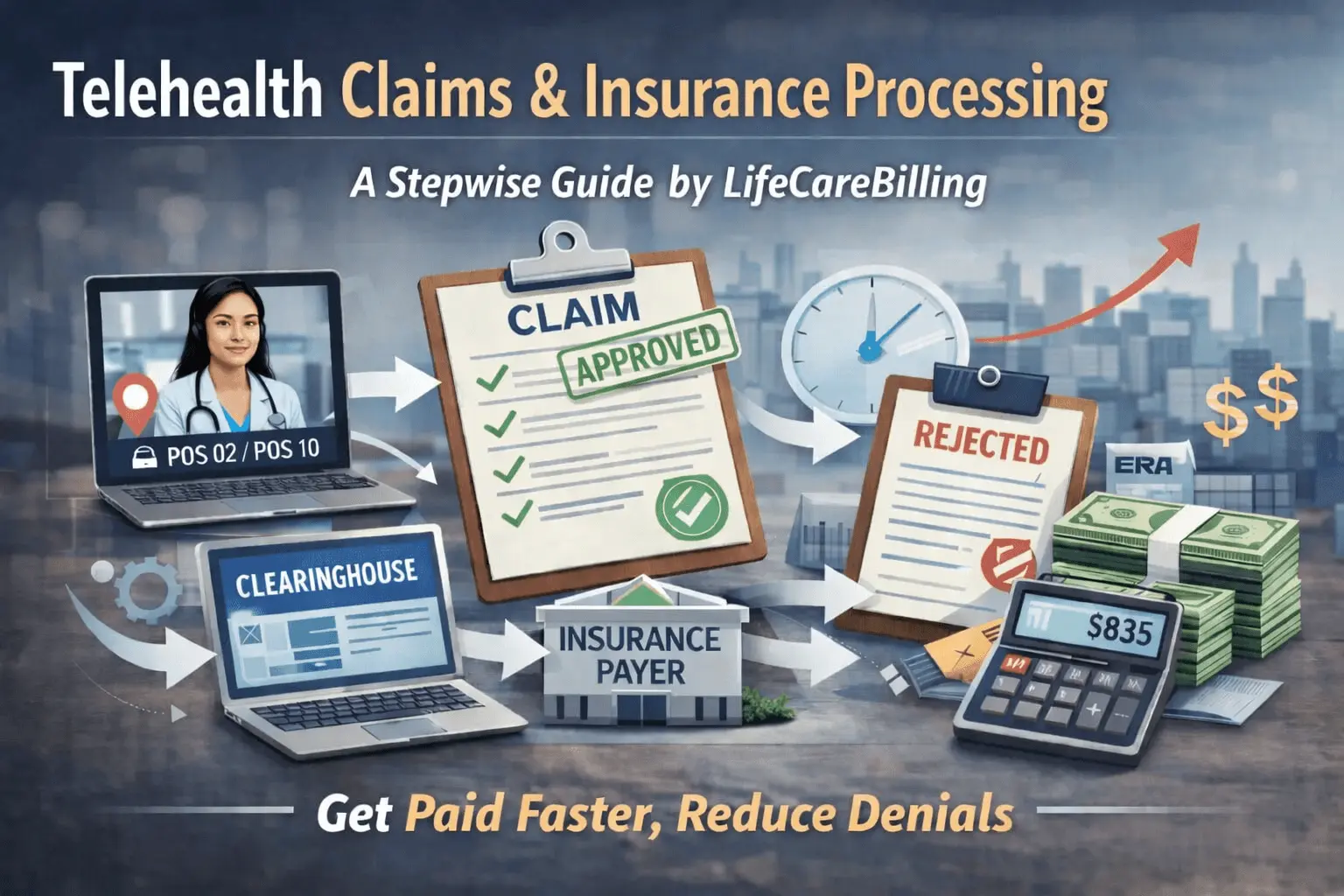
Telehealth Billing Basics for Online Doctor Visits – LifeCareBilling
Your schedule is packed. Your patients love telehealth. So why do your payments still feel... unpredictable?
If you're wondering why claims get paid this week but denied next week—even when you're doing the same thing—the problem usually isn't your clinical care. It's your telehealth billing workflow.
For patients, telehealth is beautifully simple: click a link, see their provider, get care. But behind that seamless experience? Your revenue can break for surprisingly small reasons. A wrong place of service code here. A missing modifier there. Documentation that's clinically perfect but billing-incomplete. Payer rules you didn't know changed. Enrollment issues that weren't caught upfront.
And when telehealth claims break, they don't break quietly. You get denials. Rework. Aging A/R. Cash flow stress.
At LifeCareBilling, we build telehealth revenue like a system—so you can scale virtual visits without scaling denials. We handle revenue cycle management, clean claims, compliance-first workflows, denial management, A/R follow-up, reporting visibility, and credentialing and enrollment for practices in New York (including Long Island) and providers nationwide.
Why Telehealth Claims Deny More Than They Should
Here's the thing: most denials don't actually start when you submit the claim. They start way earlier.
The patient's coverage wasn't verified for telehealth benefits—or their plan has specific setup requirements nobody checked. The provider is credentialed "in general" but not correctly linked for that payer, group, or location. The claim goes out with the wrong POS 02 or POS 10 because location logic was inconsistent. The wrong modifier gets added—or the right one gets forgotten entirely. Documentation doesn't clearly show what the payer expects to see for a telehealth encounter.
The fix isn't "try harder next time." The fix is building a repeatable billing workflow that makes telehealth claims easy to submit correctly every single time.
What "Telehealth Billing" Actually Means (In Plain Language)
Getting paid for telehealth isn't just about coding a visit. It's about matching your claim to multiple moving pieces:
Payer policy (Medicare vs commercial vs Medicaid plans all have different rules). Patient location (especially whether they're home or somewhere else). Service type (audio-video vs audio-only; E/M vs therapy vs mental health). Correct coding + place of service. Telehealth documentation requirements for that specific payer and service.
CMS reminds providers that place-of-service coding describes where services were rendered and that reimbursement policies can vary by payer. Translation? Your workflow needs to be payer-aware, not guess-based. (Centers for Medicare & Medicaid Services)
The 5 Decisions That Determine Whether Your Telehealth Visit Gets Paid
Think of every telehealth visit as running through a quick "billing decision tree." Get these five steps right, and telehealth stops feeling random:
- Is the patient eligible? Is telehealth covered under their plan today?
- Where is the patient located? Specifically: are they at home or somewhere else?
- Is the provider properly enrolled? Are you linked correctly with the payer for telehealth services?
- What POS code should be used? POS 02 or POS 10?
- What modifier should be used? Modifier 95 (audio-video) or modifier 93 (audio-only), or something payer-specific?
Standardize these five decisions, and telehealth billing becomes predictable.
POS 02 vs POS 10: The Most Common Telehealth Billing Mistake
This is where a lot of practices quietly lose money.
What They Actually Mean
HHS makes it clear for Medicare Fee-for-Service claims:
- POS 02 = telehealth provided other than in the patient's home
- POS 10 = telehealth provided in the patient's home (telehealth.hhs.gov)
CMS updated the POS code set specifically to support this distinction, including adding POS 10 and revising POS 02. (Centers for Medicare & Medicaid Services)
Why It Matters Financially
Here's where it gets expensive. CMS guidance explains that Medicare pays telehealth differently based on POS:
- POS 02 is paid at the facility rate
- POS 10 is paid at the non-facility rate (Centers for Medicare & Medicaid Services)
So if you're billing POS 02 when the patient is actually at home—or your workflow just defaults incorrectly—you could be leaving money on the table. Or creating claim inconsistencies that trigger payer reviews.
LifeCareBilling approach: We build simple, rule-based workflows so "patient location → correct POS → clean claim" happens automatically in your process. No guessing at submission time.
Modifier Basics: When to Use Modifier 95 vs Modifier 93
Modifiers are signals to payers. They tell the insurance company exactly what kind of telehealth service was performed.
Modifier 95 (Audio-Video)
Modifier 95 is commonly used for real-time interactive audio-and-video telemedicine services. Payer rules vary, so your workflow must follow the specific plan or MAC guidance. Medicare Administrative Contractors publish their own telehealth modifier guidance and expectations. (novitas-solutions.com)
Modifier 93 (Audio-Only)
The AMA describes modifier 93 as being used for audio-only services—basically telephone or voice-based services when applicable. (American Medical Association)
The AAFP also notes using modifier 93 for audio-only services and highlights that payer adoption varies significantly, especially between Medicare and other payers, and in settings like FQHCs and RHCs. (AAFP)
The Important Reality
Audio-only rules are one of the most payer-specific areas in telehealth. Even within New York, different agencies and payers publish their own specific instructions. For example, NY OMH has audio-only modifier guidance for certain OMH services. (omh.ny.gov)
LifeCareBilling approach: We don't guess modifiers. We standardize payer rules into your billing playbook, then run claims through clean checks before submission.
Telehealth Documentation Requirements: What You Must Capture Every Time
APPs, physicians, and telehealth-first clinics all run into the same frustrating problem: their clinical notes are perfectly fine, but billing reviewers want something more specific.
Here's the documentation baseline that keeps telehealth claims defensible:
- Patient consent (when required by payer or practice policy)
- Date of service and type of telehealth (audio-video vs audio-only)
- Patient location (home vs other)—this directly supports correct POS logic
- Provider location (if your payer requires it)
- Time (if billing is time-based) or clear MDM support (if billing by medical decision-making)
- Chief complaint, assessment, plan, and any orders
- Any technology or connection issues that affected the visit (even just a quick note)
- If coordinating care: who you communicated with and why it mattered
Why This Reduces Denials
It prevents "documentation mismatch" denials that force you into rework and appeals later. Your note tells the full story upfront.
Medicare vs Commercial vs Medicaid: The One Rule You Can Always Trust
There's one rule about telehealth billing that never changes:
Telehealth billing rules vary by payer.
Even CMS emphasizes using POS codes correctly and checking payer reimbursement policies and guidance. (Centers for Medicare & Medicaid Services)
So your workflow should be built around three clear pathways:
- A clear Medicare pathway (POS + modifier rules)
- A clear commercial pathway (often different modifier rules and telehealth policies)
- A clear Medicaid/state-specific pathway (policy can vary significantly)
This is why "telehealth billing basics" isn't just about education—it's about operational design.
Common Telehealth Billing Denials (And What Actually Fixes Them)
Here are the denial patterns we see most often:
Wrong POS: Patient at home but billed as POS 02 instead of POS 10, or inconsistent location logic (telehealth.hhs.gov)
Missing or incorrect modifier: Modifier 95 or modifier 93 missing when required (American Medical Association)
Patient eligibility not verified: Telehealth benefits weren't confirmed, or plan limitations were ignored
Provider enrollment incomplete: Not fully credentialed or not linked correctly (group/NPI mapping issues)
Documentation doesn't clearly support telehealth method: Especially for audio-only services (American Medical Association)
Claims sent without consistency: EHR and billing system location/modality fields don't match
LifeCareBilling fix: We run telehealth through a repeatable pre-claim process: eligibility check + enrollment verification + claim scrub + denial tracking + weekly A/R routines.
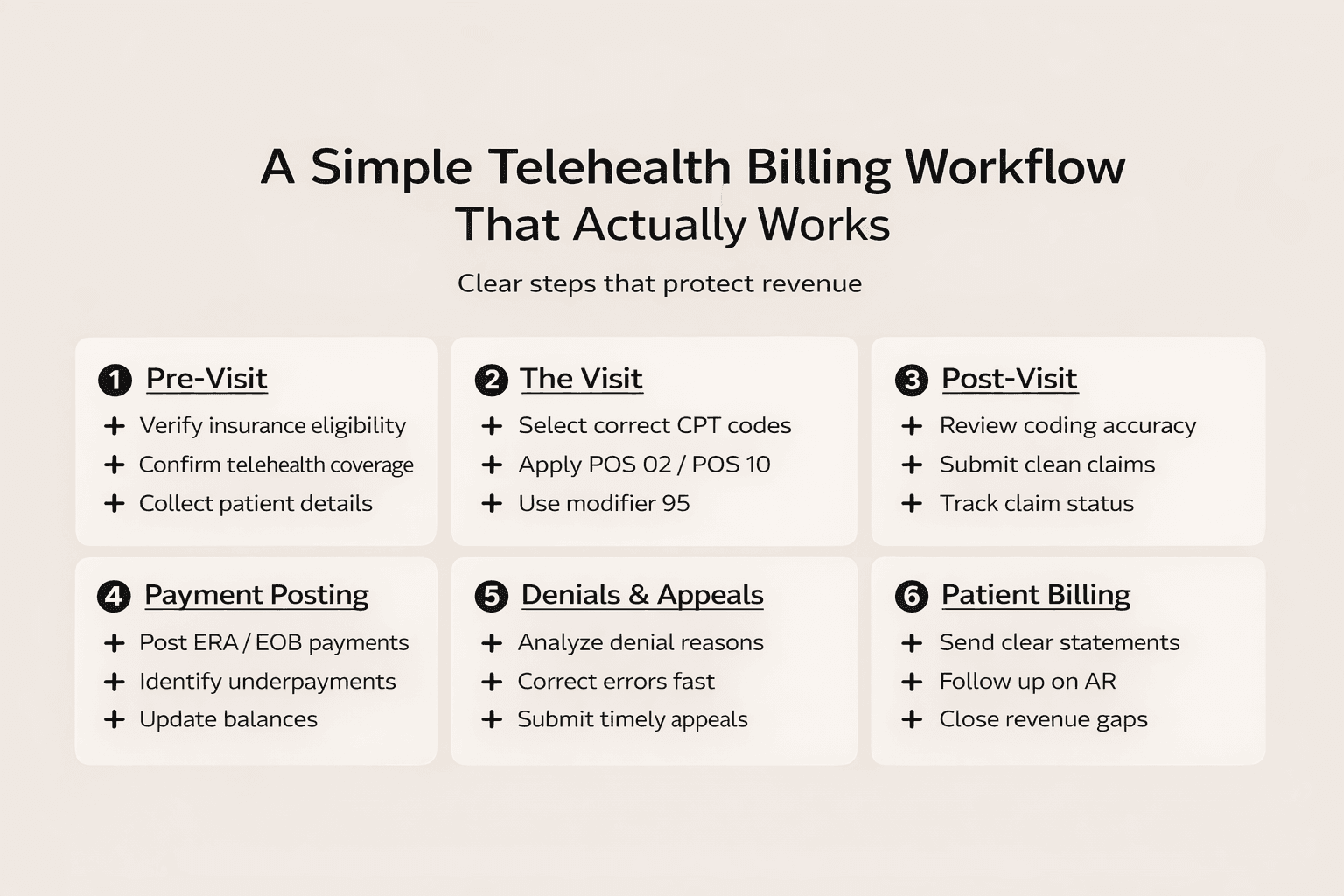
A Simple Telehealth Billing Workflow That Actually Works
Step 1: Pre-Visit (Build Clean Claims Before the Visit Even Happens)
- Confirm eligibility and telehealth coverage
- Confirm the patient's expected location at time of visit (home vs other)
- Confirm payer rules for modifiers and POS
Make sure provider enrollment and credentialing is active and properly linked
Step 2: During Visit (Capture What Billing Needs Without Slowing Down Care)
- Note modality (audio-video vs audio-only)
- Document location and medical necessity/MDM (or time, if billing time-based)
- Keep the note simple, consistent, and complete
Step 3: Post-Visit (Submit Clean, Track Fast, Fix Root Causes)
- Submit correct POS (POS 02 or POS 10) (telehealth.hhs.gov)
- Apply correct modifier (modifier 95 or modifier 93) when required (American Medical Association)
- Track denials by reason and repair the workflow—not just the individual claim
- Follow A/R consistently until payment is closed
Telehealth Billing for Growth: What Breaks When Volume Increases
Telehealth scales fast. That's the beautiful part. It's especially powerful for:
- Primary care
- Behavioral health
- Chronic care follow-ups
- APP-led practices
- Telehealth startups
But here's what happens when volume increases without workflow tightening:
- You add new payers without updating billing rules
- You expand multi-state without tightening enrollment and compliance
- Your documentation becomes inconsistent across multiple providers
CMS telehealth resources and MLN guidance are updated regularly (including telehealth and remote patient monitoring topics), so practices need ongoing monitoring—not a one-time setup. (Centers for Medicare & Medicaid Services)
Telehealth Billing Services in New York, Long Island, and Nationwide
If you're searching for telehealth billing services, telemedicine billing services, telehealth billing company near me, telehealth billing Long Island, telehealth billing New York, outsourced telehealth billing, or telehealth revenue cycle management—this is exactly what we build.
LifeCareBilling operates from Commack, NY and supports providers and clinics nationwide with end-to-end billing and RCM, plus credentialing and reporting support. (lifecarebilling.com)
What You Get with LifeCareBilling
- Telehealth billing workflows built for POS + modifier accuracy
- Eligibility and benefits verification routines
- Clean claim submission and coding support
- Denial management, appeals, and root-cause fixes
- A/R follow-up that prevents revenue leakage
- Credentialing and enrollment tracking so growth doesn't get blocked by admin issues
- Reporting visibility so you know what's paid, what's pending, and why (lifecarebilling.com)
- Call (631) 966-1755 or click Get Free Billing Analysis to see what's working, what's leaking revenue, and how to stabilize telehealth payments. (lifecarebilling.com)
Frequently Asked Questions
What are telehealth billing basics?▼
Telehealth billing basics means billing virtual visits correctly by matching payer rules with the right POS code, modifier, and documentation so claims pay predictably.
What's the difference between POS 02 and POS 10?▼
For Medicare, POS 02 is telehealth provided other than in the patient's home, and POS 10 is telehealth provided in the patient's home. (telehealth.hhs.gov)
Does POS 02 vs POS 10 change payment?▼
Yes. CMS guidance explains Medicare pays POS 02 at the facility rate and POS 10 at the non-facility rate. (Centers for Medicare & Medicaid Services)
When do I use modifier 95?▼
Many payers use modifier 95 to identify synchronous telemedicine services. Always follow your payer or MAC instructions because modifier requirements vary. (novitas-solutions.com)
When do I use modifier 93?▼
Modifier 93 is used for audio-only services when applicable. Payer rules vary significantly. (American Medical Association)
How does LifeCareBilling help telehealth providers?▼
LifeCareBilling supports telehealth providers with billing and RCM workflows, credentialing support, denial prevention, A/R follow-up, and reporting dashboards—so telehealth growth doesn't turn into denial growth. (lifecarebilling.com)

 Back to Blog
Back to Blog December 31, 2025
December 31, 2025